- Investment follows strong employer and health plan demand as substance use management moves from niche solution to essential benefit resulting in 287% revenue growth in 2023 and 100% client retention
- Growth follows 500% increase in substance use disorder-specific RFPs from employers and payers in the past twelve months
- Platform covers more than 3.4 million eligible lives
NEW YORK–(BUSINESS WIRE)–Pelago, the leading digital clinic partner to U.S. businesses and health plans for substance use management, today announced $58 million in new funding on the strength of customer growth and validated ROI, bringing total funding to $151 million.



The additional capital raised will help Pelago accelerate its product roadmap, extend its continuum of care and advance clinical research efforts. Existing investor Atomico doubled down to lead this Series C investment on the back of Pelago’s impressive growth, with participation from all existing investors Kinnevik AB, Octopus Ventures, and Y Combinator plus new investors Eight Roads and GreyMatter Capital. As part of this latest round, Atomico Partner Laura Connell will join the Pelago board.
“I’m so proud of the work we have done to improve lives and expand access to substance use care that works. We empower employers and payers to bring our solution to their members struggling with tobacco, alcohol or opioids, from prevention to treatment and recovery,” said Pelago CEO and Co-Founder Yusuf Sherwani, M.D. “We’re addressing a gap in the market left by employee assistance programs and mental health benefits providers who are unable to detect and treat substance use disorders. Customers are resonating with our solution as evidenced by a tenfold growth in revenue and eligible lives since our Series B two years ago.”
Pelago was founded on the premise that substance use is a treatable chronic condition. The company is addressing the rising rates and costs of substance misuse head-on through its 100 percent fees-at-risk model that delivers improved outcomes and demonstrated ROI. In the industry’s first ever substance use management medical claims analysis, Pelago’s substance use management program reduced medical claims on an annual basis by $9,367 per participant compared to a control group, delivering a 3.0x ROI. More than 80 percent of cost savings realized in the Pelago analysis were attributable to lower medical spend, with the remainder tied to lower behavioral health costs.
“Yusuf and the Pelago team are building the category-defining company in substance use management and in doing so, addressing one of this generation’s most urgent healthcare needs,” said Atomico Partner Laura Connell. “Their visionary leadership in the substance use management space, in offering treatment as an employee benefit to the world’s most forward-thinking companies, is reflected in their exceptional growth, testament to the significant and rapidly growing demand for better solutions. Pelago’s ability to expand and accelerate access to best-in-class substance use care results in a major improvement in clinical outcomes and costs with clear and material ROI for employers. Atomico is incredibly proud to have supported the Pelago team on the journey thus far and to be doubling down on our partnership now.”
With rapidly rising healthcare costs, employers and health plans are laser-focused on value, cost-savings, and performance-based care for their employee and member benefits. According to recent surveys from consulting firms Mercer and WTW, costs for workplace health plans in 2024 will jump more than 6 percent. Moreover, recent Centers for Disease Control and Prevention research has reported the annual minimum direct cost of substance use disorders (SUDs) at $15,640 per affected employee enrolled in employer-sponsored insurance, totaling more than $35 billion annually.
In non-specialized SUD treatment settings, research shows up to 89% of adults with SUDs may go undetected, resulting in delays in treatment, relapse and increased costs. And for those that do receive SUD treatment in mental health settings – the treatment itself is not the specialized SUD treatment they need. All the while, the consequences in terms of hidden financial and productivity impacts remain buried in medical claims and absenteeism, dramatically impacting a company’s bottom line in the form of costly health problems, inpatient and outpatient care, poor utilization management and lower productivity.
“As a company that provides our employees with a broad range of health, life and voluntary benefits, Live Nation Entertainment is proud to offer Pelago’s value-based, substance use management benefit,” said Emily Munroe, Director, Benefits for Live Nation Entertainment. “I congratulate Pelago on its funding raise, and I look forward to a continued strong relationship with their entire team.”
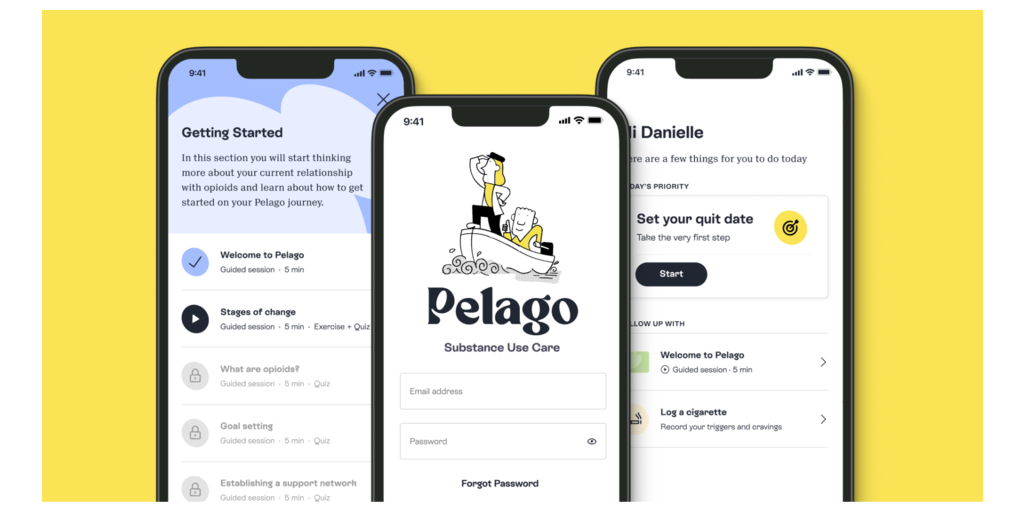
Pelago offers integrated substance use management to employer and health plan populations, with specialized treatment for tobacco, alcohol and opioid use disorders along with support for adolescents. For more information, visit www.pelagohealth.com.
About Pelago
Pelago partners with enterprises as the leading virtual clinic for substance use management among their employees. We are transforming substance use support – from prevention to treatment – delivering education, management skills, and opportunities for positive change to members struggling with substance use, most commonly tobacco, alcohol or opioids. Our solution gives employers the means to offer on-demand, personalized support to workers seeking to live healthier lives. Pelago’s cognitive behavioral therapy (CBT) and medication-assisted treatment (MAT) programs deliver convenient, accessible and effective support that seamlessly integrates with health plans, pharmacy benefit managers and wellness platforms. Tens of thousands of members enroll in the Pelago program each year, and more than 3.4 million now have access to the digital clinic.
Contacts
Bruno Solari
bruno@solcomms.co
303-335-9180




